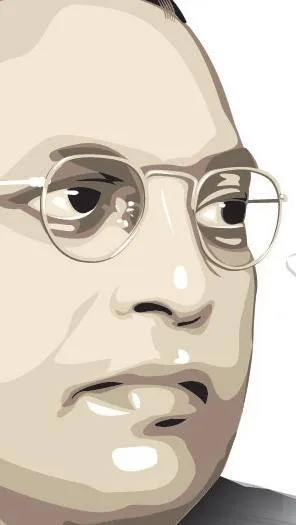
Dr. Sylvia Karpagam
 (Critique of the model of Universal Health Coverage in Karnataka – response to an article, ‘Bogeys on the Universal Health Coverage train‘, in the Hindu on July 28th 2016)
(Critique of the model of Universal Health Coverage in Karnataka – response to an article, ‘Bogeys on the Universal Health Coverage train‘, in the Hindu on July 28th 2016)
K Srinath Reddy has been allowed prime space under policy watch by the Hindu, dated 28th July 2016, to share his thoughts and deep understanding of the health system in the country. While warning us that the public health agenda should not be derailed by the populism of electoral politics, personal preferences of prominent medical professionals or the parsimony of public financing, he then goes on to talk about a revamped Rashtriya Swasth Bima Yojana without even having the ethics to talk about the serious issues arising out of this scheme.
The Parliamentary standing committee in its 92nd report raised serious concerns about the Medical Council of India (MCI) on its failure to connect medical education with the health system and to create a curriculum that produces doctors suited to working in the Indian context especially in the rural and poor urban areas. The devaluation of merit in admission, especially into private medical institutions and particularly due to capitation fees, has made medical education available only to the rich and has failed to produce competent basic doctors. The report also states that there is heavy focus on infrastructure without substantial evaluation of quality of teaching, training or imparting of skills, and a failure to put in place robust quality assurance mechanisms for practicing doctors. There has been a failure to create transparent systems of medical college inspection and granting of recognition or de-recognition. The MCI has failed to oversee and guide the Continuing Medical Education in the country, leaving this important task to the hands of the commercial private industry. There is a failure to instil respect for a professional code of ethics in the medical professionals and take disciplinary action against doctors found violating the code of Ethics.
One needs to look no further than the pitiable state of affairs of health care in Karnataka to comprehend the level of damage that health care providers and policy makers have inflicted. The pro-privatisation bias of policy makers and the wilful denial of care and negligence displayed by private and public service providers will only pave the way for further deterioration of the health situation. While government policy makers pat their own backs after generating fraudulent reports of their own performance, the private players are even more evolved in that they generate no reports and are accountable to nobody. The Medical Council of India, the Karnataka Medical Council and all regulatory bodies are dysfunctional and deliberately dis-involved.
The Universal Health Coverage as propagated by the Public Health Foundation of India (PHFI) is a blueprint of this large scale decay of health service provision. The language of the program, initiating with the recommendations of the High Level Expert group has been gaining momentum and has found its fertile roots in Karnataka, supported as it is by a apathetic public health system and a voracious corporate and business mafia.
The language of the document on UHC is fraught with innuendo, readily moving from rhetoric to empty and false promises, manipulating information to blatantly suit its own vested interest and that of the business mafia waiting to enter mainstream healthcare.
The UHC program has moved from the language of ‘free ‘healthcare to ‘affordable’ healthcare. When there is no political commitment to making health a fundamental right in India and in the absence of such a legal enforceable right, the UHC deliberately lays itself bare to be hijacked by vested interests. The term Universal Health Coverage itself, while meaning different things in different countries based on their political will and commitment to comprehensive health care, is open to manipulation. While PHFI quotes the example of Thailand’s UHC, it fails to disclose that the model that Thailand has chosen is in principle very different from that being suggested for India. Therefore under the umbrella term of UHC and quoting various functioning models of other countries, PHFI is fraudulently attempting to introduce a pro-private model of healthcare.
On the front of transparency and accountability, PHFI holds a poor record. Since its inception the organisation has been in the limelight for all the wrong reasons. Queries have been raised about the composition of the ‘founding’ members (sometimes 8, sometimes miraculously doubled to 16, sometimes 24). The organisation has been accused of fraud and forgery. An RTI application filed in 2005 was responded to with forged documents and unlawful interference in the statutory role of a PIO. Dr. Srinath Reddy, who has given AIIMS as his official id is prohibited by the rules of government employees to participate in the formation of an organisation such as PHFI and to solicit funds and neither has he received any authorisation from a public authority to do the same. In a similar bypass of protocols, the High Level Expert Group, seemingly a government body, is conveniently housed in PHFI, which incidentally also houses the Bill and Melinda Gates office, that ‘voila’ has recently been under the radar for ‘influencing government health policies in favour of multinational pharmaceutical companies. One therefore realises that the credentials for being part of the esteemed PHFI/BMGF collaborative and colluding nexus, are not a strong background in public health but an inerring ability to flex power, influence policy, twist evidence and stand by a pack of lies, inspite of all evidence to the contrary. The innumerable criticism of PHFI in the public domain would surely not be lost on the government. One can therefore reasonable assume that the government is willingly and wantonly handing over healthcare to PHFI, to wreak havoc as it wishes.
Sujatha Rao, who was the Health Secretary in the Government of India has come down heavily on the health insurance model (Rao, 2014). She gives evidence from the state of Andhra Pradesh that initiated the Rajiv Arogyashree Health Insurance scheme (RAS), one of the first state led health insurance programs in the country. She says that the State ‘consciously chose to abandon primary care for universal coverage of a select set of tertiary and secondary care conditions’. The RAS was critiqued as having boosted the revenue streams of private corporate hospitals without necessarily reducing health expenditure or improving health outcomes. The percentage of those incurring catastrophic expenditure more than doubled from 1.1% to 2.8% and 1.2% to 3.4% for the two lowst quintiles of population mainly due to concentration of half the accredited hospitals in seven towns leading to inequitable distribution of and gross deficiencies in the supply side, making access difficult and unaffordable for those residing in backward areas. This very same finding has been documented by none less that Institute of Social and Economic Change (ISEC), a government supported organisation which shows that out of pocket expenditure has gone up with the Stat sponsored insurance schemes, access has decreased and concentration of cases in towns, with four hospitals in Bangalore bagging the lion’s share of the reimbursements. In Andhra Pradesh, cardiac cancer and kidney disease have seen the maximum referrals while the bottom two quintiles in reality suffered from premature mortality and disability due to lower respiratory infections, diarrhoeal diseass, tuberculosis, ischemic heart disease and malaria – conditions ’eminently preventable and treatable with effective primary care. The appointment of Dr. Devi Shetty as the Health ombudsman and in the Board of the Suvarna Arogya Suraksha trust (SAST) for implementation of the Vajpayee Arogyashree when his chain of hospitals receive the major share of reimbursements under the very same scheme, reeks not only of vested interest but arrogance and impunity of these corporate entities and their ever willing and colluding government counterparts that they have zero accountability to anyone.
Sujatha Rao also writes about how the introduction of health insurance schemes in Andhra Pradesh was the death knell for the primary health care system and that AP was the only state that had slashed its primary care budget from 53% to 46% and allocate just 9% for secondary care down from 12% during 2007-12. Not surprisingly, RAS was provided 23% of the health budget covering less than 1% of the population and not necessarily the poor. She says that prices were set through negotiations with private hospitals by committess without professionals and that package rates provided scope for gaming the system. ‘In the absence of standards to measure quality and regulation to control provider behaviour and fraud, perverse incentives are created, as reflected in unnecessary diagnostics, procedures and surgeries.”
Since Sujatha Rao has clearly stated the anti-people effect of health insurance schemes, several states have documented in several peer reviewed journals, the wilful denial of care, negligence, cherry picking, unwanted procedures and investigations that patients, many of them women and from extremely marginalised communities, have been subjugated to. That bodies such as PHFI, that lay stakes on policy making and research, should wilfully ignore these reports and continue to promote these very same schemes to a pitifully submissive health department in Karnataka, shows their virulent disregard for people’s health and a single minded agenda of opening up the playing field for private players while actively breaking down the public health system.
The presence of Rajat Kumar Gupta on the board of PHFI begs certain questions. Why should a former global managing director of McKinsey and Co and Goldman Sachs be on the health policy making board for the country? McKinsey is an American company that sells its service to open markets and towards insurance while Goldman Sachs provides investment banking. What is the ethic or playing field of these kind of agencies or individuals with these backgrounds? Are we to leave the fate of our country to these kind of players who view women who enter the workforce for the first time as ‘potential buyers of health service’? Would poor women entering the work force for the first time want to spend their money for healthcare, or would they rather use the money earned out of their hard work and sweat to build better lives for their children and families? What ethic would such agencies possess that look at healthcare as a commodity and people, especially the poor, as potential ‘buyers’? Leaving aside these questions, one wonders how someone who went ahead to become a board member of PHFI, was later arrested and imprisoned for a period of two years for insider trading? Is there no requirement for board members of a body such as PHFI, which has been given such terrible powers, to possess some credibility, some experience in public health care or of having worked with people or communities? Is it really of any wonder then that policy documents such as the one released by PHFI for UHC would be emerging as such a macabre joke if it wasn’t for the fact that it is going to adversely affect the lives of people, a majority too poor to be able to resist the sea change under the guise of new policy.
Is PHFI a government initiative? Is it an autonomous body? Is it a society? Is it a public private partnership? Who is it accountable to? How are its corporate board members installed? Why are Bill and Melinda Gates their primary donors? Why is an insurance promoting American company vis a vis McKensie on the board of a public health body of the country? What are the credentials/expertise/capacity of Narayan Murthy, Founder of Infosys, to be the Chairperson of PHFI? Is health a joke that any random business tycoon be placed at its head? Of course most of these questions, are and will remain unanswered. The solution is not to look for answers but for health care to be located where such questions are not necessary.
“In December 2013, a Government Order (GO.NO: HFW171FPR 2013) was issued identifying Public Health Foundation of India(PHFI) as the technical support agency to enable the state government in drawing the basic approach for constructing the pilot projects. In addition, state level task force was also formed to provide the overall guidance, supervision and monitoring to take forward and roll out Universal Health Coverage in the selected districts.” This innocuous statement belies the fact that a dangerous trend is being manifest. Processes of tendering, monitoring, regulation and accountability have been held at bay in the context of PHFI. The health of the country has been literally handed over to this fly by night agency that sprung up suddenly, with redoubtable credentials and clear pro-market agenda. How did the government ‘issue’ such a body a government order as technical support agency? It only goes to prove the complete culpability and collusion by both state and central governments in letting a redoubtable agency to do pretty much whatever it pleases with health in the country and state. Obviously what pleases this agency is already visible for anyone with an iota of concern – destruction of the public services and unregulated rampant proliferation of greedy market mafia.
The fact that health insurance is making inroads into secondary care in Karnataka, only goes to prove that PHFI’s agenda is to directly shift patients from the closest point of contact and easiest point of access, further and further away. It is evident that the further a patient moves from his community and home, the more vulnerable he or she is to conniving private profiteerers and this eventuality is not without the conniving facilitation by PHFI and the deplorable collusion by the state government. There is ample evidence with the RSBY, VAS and Yeshaswini, and this is even documented by PFHI in their own assessment report. One would assume that the findings about these schemes would raise alarm bells in even a nominally concerned and intelligent policy maker. Apparently, with PHFI and GoK that is substantially more than one can expect.
By constantly referring to 25 top priority conditions, PHFI makes it amply clear that only those conditions that can generate income for the private sector, would even make it past the Health and Wellness centres to the secondary facility. What would happen to the 26th condition, or the 27th condition, or even the 235th condition is left to one’s imagination. PHFI seems to assume that there is no commitment by the government towards conditions other than these 25. Not surprisingly, the major conditions emerge as those of cardiac origin. Saying comprehensive health care and ‘top priority conditions’ in the same context is no more than an oxymoron and as expressed earlier, one realises that PHFI has been trained to mouth these ridiculous inanities without so much as an elementary cognition of the ludicricity of this position.
PHFI makes a loose sweeping statement that CHCs and PHCs are not ‘contributing much in delivery care”. While a serious policy maker would look at this statement with much concern, try to verify the truth of this statement and if indeed true, look for solutions to address the issue.. Instead PHFI, having showed CHCs and PHCs in a bad light, then goes on to promote the private sector, which was never even evaluated in the first place.
There is adequate evidence from studies in Karnataka to show that health insurance schemes are not reaching the poor. The number of agencies that stand to gain by health care being opened to the markets cannot be undermined or pretended to not exist. The pharma industry is a big stake holder and the Indian market would provide valuable stakes to the pharma industry. Similarly, there will be huge gains of biomedical products and equipment. These companies have aggressive marketing strategies that arm twist entire governments to change the very nature and structure of service provision. The Indian policy makers are more than ready to allow these destructive changes to take place in exchange for financial or social gain. It has been seen time and again that those agencies and individuals and organisations that stand the most to gain by certain policy changes, are the ones who are making the policy changes in the first place.
What Srinath Reddy fails to mention is that the state sponsored health insurance schemes have also been associated with poor quality of care, violation of ethics and inability of government to regulate the private sector in anyway either for quality, costs, reporting, documentation, adherence to standard treatment guidelines or humane patient care. The primary beneficiaries of this model have been the private sector, particularly those who are currently occupying key positions on various committees and commissions set up by the government. PHFI however use a twisted logic to say that because utilisation of public facilities is low and because number of private facilities are high, that private facilities should be further enhanced as the main providers. With this innate bias, PHFI deliberately misleads in favour of private service providers. At no point in the assessment report has PHFI looked even cursorily at the nature of service provision by the private providers, especially under the state sponsored health insurance schemes. That costs to patients have skyrocketed, that patient’s bodies have been violated and ravaged with unnecessary tests and unwanted procedures, that there has been fear mongering, that patients have been offered choices between poor and ‘better’ healthcare, that patients have been discharged unceremoniously without any cognizance of serious post surgical complications, that patients who fall outside the ‘package’ are made to run from pillar to post without recourse to public facilities that are being systematically disabled – why do these unacceptable violations not even figure as footnote in PHFI’s assessment report? Is this really an assessment? If yes, is it objective? Can such a report be used as a baseline to implement a policy for the state? Has not even one government official found this to be a cause for concern? Are our state policy makers so apathetic, so disempowered, so corrupt that they will not question such a blatantly biased report?
It appears that PHFI is eager to present the public health services as failing and private players as a panacea to all the woes and ailments in the health system. The solution of PHFI is ready made. Its recommendation that ‘ to overcome the limited availability of diagnostic services such as ultrasonography, CT, MRI and other advanced diagnostics in taluka hospitals, contracting out of these services to private sector facility can be attempted.”
Is it rational and objective for PHFI to be on policy making, planning, implementation and evaluation? Is there any commitment by the state to have an objective evaluation of the kind of model proposed by PHFI that is envisaging structural changes in an already vulnerable public health system. Criticisms against PHFI are easily and readily available in the public domain. Is the state government being deliberately dense or are they so dangerously naïve that they would hand over public health services to any agency with a vicious vested interest? Has the state government learnt no lessons from its previous irrational and unconstitutional engagement with private players.
To add fuel to the fire, the state government has created a para statal anti constitutional body called the Karnataka Jnana Ayoga that is comprised of business tycoons and corporate mafia who stand to greatly personally benefit from the recommendations of the committee. The Jnana Ayoga has been criticised for being an elitist body with vested interests and zero linkages to or concern about the field realities. Why then is the state government persisting on these non transparent bodies? What do these bodies have to hide that their proceedings and recommendations are beyond the reach or access of the common person? The Jnana Ayoga comprises Kiran Mazumdar Shaw whose anti-people stance has been criticised strongly in several sectors and domains. The Biocon tycoon heads a drug and biotechnology industry and has been made the co-ordinator of access to affordable medicine. The irony of this cant be lost even on the State government that is colluding with the private sector to wilfully damage the public health system while feigning ignorance about all the consequences on people, particularly the marginalised.
~~~
Dr Sylvia Karpagam is a public health doctor and researcher. Her own experiences of pervasive and insidious brahmanical discrimination informs her critique and she would like to use all the skills she possesses to fight caste and its manifestations as part of the larger movement of dalit bahujan friends and family. She is born from an inter-caste marriage between an adi – dravida father and naidu mother.